In conjunction with the National Institute on Drug Abuse-Clinical Trials Network (NIDA-CTN), Bizzell announces the availability of three educational videos for healthcare providers managing opioid use disorder (OUD). The first two videos are animations that discuss overdose prevention. The third video is an interactive tool used to educate healthcare providers on OUD in an emergency setting.
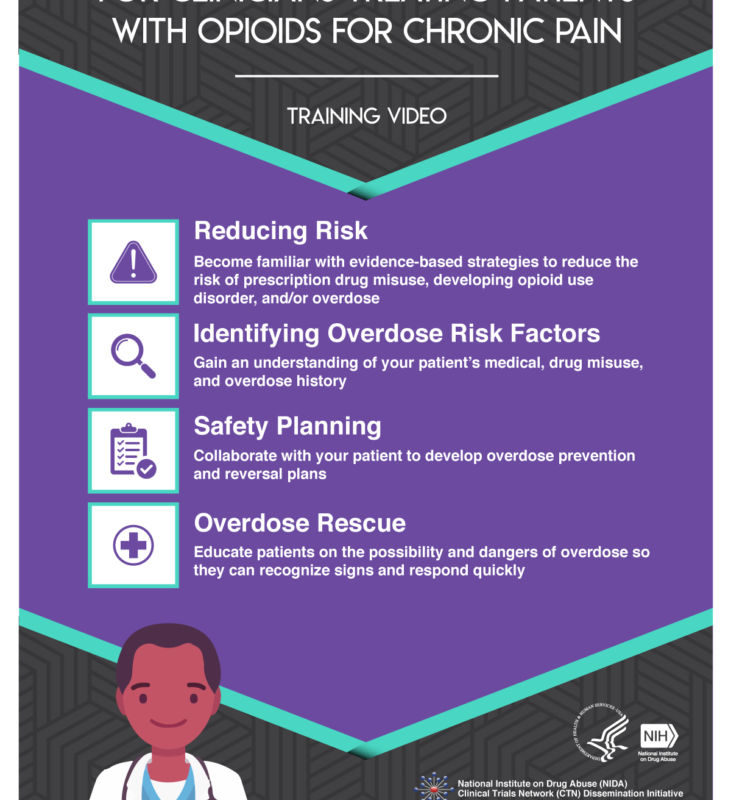
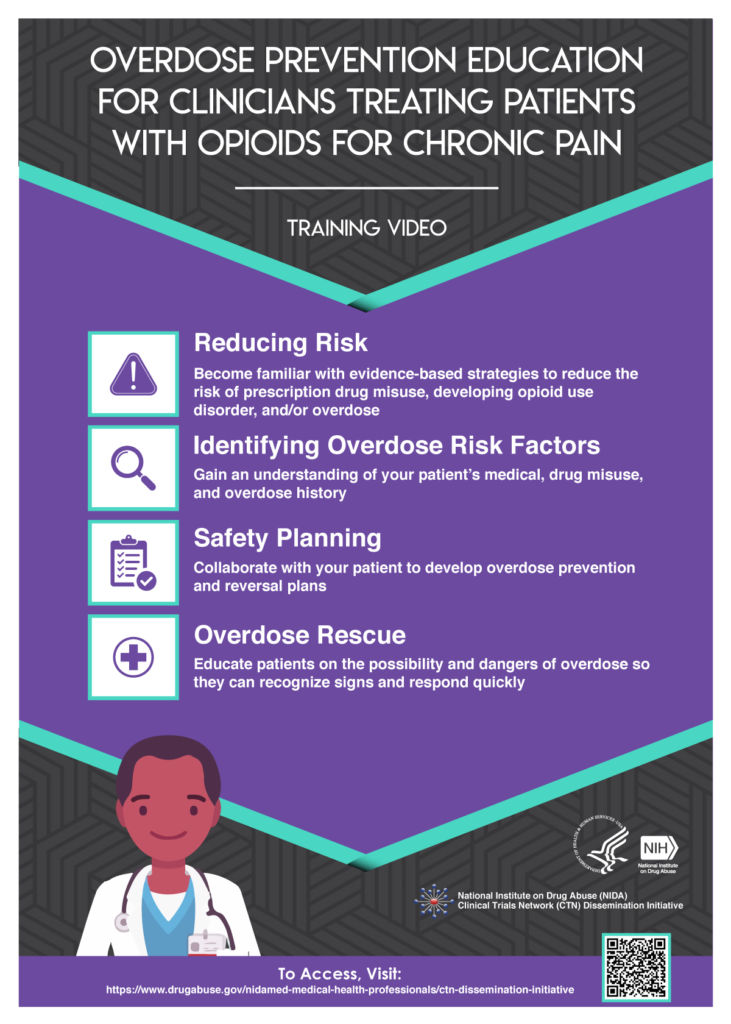
Video 1: Overdose Prevention Education for Clinicians Treating Patients with Opioids for Chronic Pain is an animated video that focuses on four key strategies: Reducing Risk for Development of OUD and Avoidance of Misuse, Identification of Risk Factors, Safety Planning, and Overdose Rescue Preparation.
Video 2: Overdose Prevention Education for Clinicians Treating Patients for an Opioid Use Disorder is an animated video that highlights three key strategies: Identifying Overdose Risk Factors, Developing a Safety Plan, and Overdose Rescue Preparation.
“These teachings are done in a simple, non-judgmental fashion offering the viewer clear and memorable points in assessing and managing opioid overdoses,” says Douglas L. Gourlay, M.D., MSc., FRCPC, FASAM, Former Director of the Pain and Chemical Dependency division of the Wasser Pain Management Centre at Mount Sinai Hospital in Toronto, a reviewer of the video.
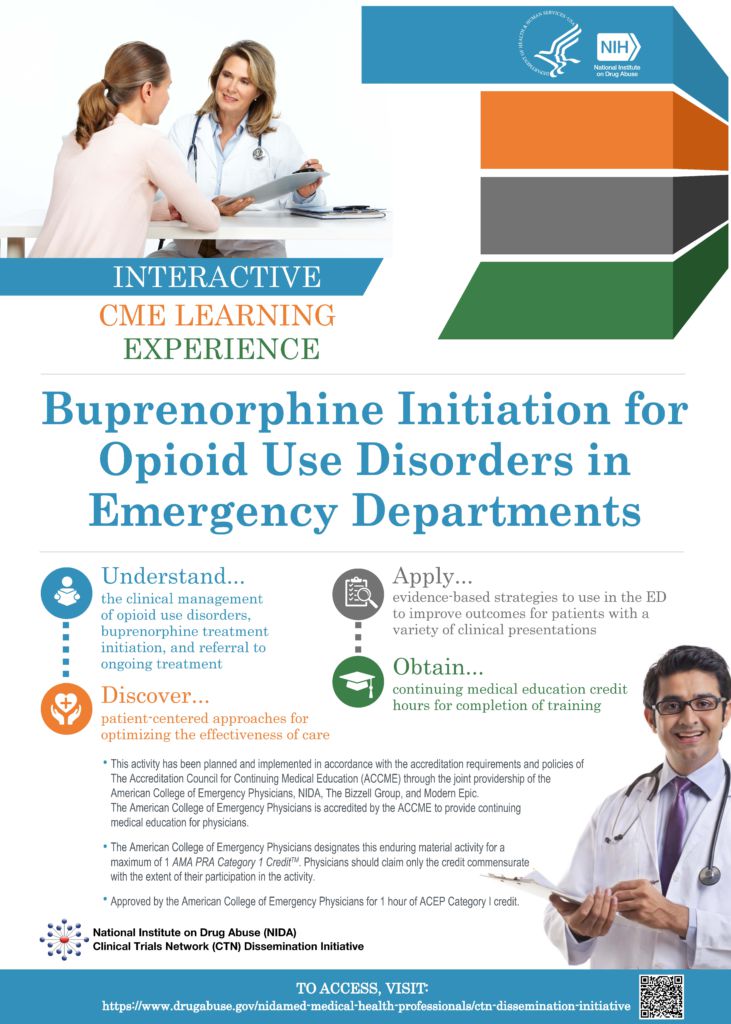
Video 3: Buprenorphine Initiation for Opioid Use Disorders in Emergency Departments: Interactive Case Vignettes is a branching video, which is an interactive educational tool. It allows participants to select a healthcare track which results in varying outcomes. The American College of Emergency Physicians (ACEP) is providing Continuing Medical Education (CME) credit and access to the tool will require the creation of a free ACEP account. Throughout the course, guidance is provided on the clinical management of OUD with a focus on screening, enlisting the patient’s input into their treatment, buprenorphine initiation, and referral to ongoing treatment.
After watching these videos, participants will be able to apply a patient-centered, shared decision-making approach while discussing the prevalence of overdose and the process of introducing buprenorphine in the ED for treatment of OUD. Participants will also be able to discuss chances for recovery as research suggests that patients are twice as likely to enter addiction treatment and remain in treatment at 30 days if medication is initiated in the ED.
The targeted audiences for the buprenorphine initiation video include: Emergency Physicians, Emergency Nurses, Nurse Practitioners, Residents, Medical Students, Physician Assistants, Emergency Department Medical Directors, Hospital Administrators, EMTs/Paramedics, and other healthcare providers engaged in the practice of emergency medicine.
“This branching video effectively and quickly walks users through the most high-yield information in the most engaging way possible. Providers around the country should see this video before their next shift caring for patients with opioid addiction,” says video reviewer, Alister Martin MD, MPP, Faculty – Center for Social Justice and Health Equity, Harvard Medical School, Massachusetts General Hospital Emergency Department.
All of the above mentioned videos were funded in part with federal funds from the National Institute on Drug Abuse, Center for the Clinical Trials Network Dissemination Initiative (contract # HHSN271201700059C). The content for the videos was developed by researchers and experts and does not necessarily reflect the official position of the National Institute on Drug Abuse, National Institutes of Health, Department of Health and Human Services, nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government. These training resources should not be considered as a substitute for individualized patient care and treatment decisions.
- This activity has been planned and implemented in accordance with the accreditation requirements and policies of The Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the American College of Emergency Physicians, NIDA, The Bizzell Group, and Modern Epic. The American College of Emergency Physicians is accredited by the ACCME to provide continuing medical education for physicians.
- The American College of Emergency Physicians designates this enduring material activity for a maximum of 1 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate .with the extent of their participation in the activity.
- Approved by the American College of Emergency Physicians for 1 hour of ACEP Category I credit.
ABOUT BIZZELL
Established in 2010, The Bizzell Group (Bizzell) is a U.S. Small Business Administration (SBA) 8(a) certified strategy, consulting, and technology firm that specializes in program management, administrative support, communications and outreach, conference management and logistical support, health services and research, technical assistance, and training and development. Bizzell’s expert staff and consultants work on health, scientific, education, environmental, research, and information technology projects that advance national priorities. Under the leadership and vision of founder, Anton C. Bizzell, MD, the company has grown from a staff of two in one small office, to a thriving firm with three offices in Lanham, MD, Rockville, MD, and Atlanta, GA, with ongoing projects around the world. Learn more about how we develop data- driven, research-informed, innovative solutions to complex-real-world challenges: www.BizzellUS.com.
ABOUT THE NATIONAL INSTITUTE ON DRUG ABUSE (NIDA)
The National Institute on Drug Abuse (NIDA) is a component of the National Institutes of Health, U.S. Department of Health and Human Services. NIDA supports most of the world’s research on the health aspects of drug use and addiction. The Institute carries out a large variety of programs to inform policy, improve practice, and advance addiction science. Fact sheets on the health effects of drugs and information on NIDA research and other activities can be found at www.drugabuse.gov, which is now compatible with your smartphone, iPad or tablet. To order publications in English or Spanish, call NIDA’s DrugPubs research dissemination center at 1-877- NIDA-NIH or 240-645-0228 (TDD) or email requests to drugpubs@nida.nih.gov. Online ordering is available at drugpubs.drugabuse.gov. NIDA’s media guide can be found at www.drugabuse.gov/publications/media-guide/dear-journalist.